
Delve into the significance of PsA outcome measures
Measuring disease activity: Composite vs individual domain measures
Disease outcome measures in PsA
Assessment of patients with PsA requires consideration of all disease domains, as well as the impact on pain, function, quality of life, and structural damage. Comorbidities and related conditions should be considered for their impact on management approaches.1
Several different measures of disease activity in PsA have been developed, including composite and domain-specific assessments2-4:
- Routine use of disease activity measures in clinical practice needs to be implemented to help more patients achieve personalized disease outcome goals1,3
- ~90% of clinicians agree that there is a need for a continuous composite measure for routine practice3
Composite disease outcome measures
Composite measures allow for the estimation of overall disease activity and disease burden across several disease domains and often include factors that are important to both clinicians and patients3,5:
- Domain severity (arthritis, enthesitis, dactylitis, axial disease, and psoriasis)
- Patient assessments of pain and fatigue
- Physical functioning assessments
- Health-related quality of life scores
Many different composite outcome measures are available, and their use in clinical practice often depends on clinician and patient preference, time available, and ease of use.2
Routine use of DAPSA and the MDA index is recommended by GRAPPA and OMERACT, and PsAID-12 (a patient-reported measure) is commonly used in clinical practice to understand the impact of PsA from the patient perspective.5,6,*
*Examples of commonly used disease measures and not an exhaustive list of all available measures.


LECTURE SERIES WITH DR. ALEXIS OGDIE
Explore 3 common composite outcome measures for PsA
In this video, Dr. Alexis Ogdie gives her expert insights on composite outcome measures that are useful for both research and a clinical setting, and how measuring many aspects of PsA together can help inform treatment decisions.
Disease Activity Index for Psoriatic Arthritis (DAPSA)
DAPSA is a GRAPPA and OMERACT guideline–recommended, validated composite measure that consists of five items: SJC66, TJC68, PtGA VAS, patient pain VAS, CRP.6-8,*
*If CRP is not included, it is called the clinical or cDAPSA (4 items).2
Considerations
- Quick and easy to administer and calculate during the clinic visit2
- Can measure both current disease activity and treatment response2
- Useful to assess polyarticular peripheral arthritis2
CRP=C-reactive protein; PtGA=patient global assessment; SJC=swollen joint count; TJC=tender joint count; VAS=visual analog scale.
Minimal Disease Activity (MDA) Index
MDA index is a GRAPPA and OMERACT guideline–recommended, validated composite measure that consists of seven items: SJC66, TJC68, patient global assessment (PtGA) VAS, patient pain VAS, enthesitis, function (HAQ), skin (PASI or BSA).6,9,10
Considerations
- Simple and easy to administer; paper or electronic applications available2,6
- MDA (and VLDA) criteria are useful measures of good disease control; a continuous measure of disease activity2
- Valid in polyarticular and oligoarticular disease2
BSA=body surface area; HAQ=Health Assessment Questionnaire; PASI=Psoriasis Area Severity Index; PtGA=patient global assessment; SJC=swollen joint count; TJC=tender joint count; VLDA=very low disease activity.
Psoriatic Arthritis Impact of Disease (PsAID)-12
PsAID-12 is a composite measure to specifically assess the impact of PsA from the patient’s perspective.11 It includes 12 physical and psychological domains: pain, fatigue, skin, work and/or leisure activities, function, discomfort, sleep, coping, anxiety, embarrassment, social life, and depression, all assessed by patients on NRS.11
Considerations
- The 12-item scale was developed for clinical practice; it is a quick, self-administered questionnaire on paper or electronic format available from EULAR2
- Correlates well with MDA/VLDA6,11,12
EULAR=European Alliance of Associations for Rheumatology; MDA=minimal disease activity; NRS=numerical rating scale; VLDA=very low disease activity.
Additional disease outcome measures in PsA
PsA is a highly heterogeneous disease and, as a result, a large array of disease outcome measures have been developed and validated to define and monitor it.2,14 These include physician- and patient-administered measures, composite and single-domain measures for each of the disease domains, and measures for quality of life and ability to carry out activities of daily living.2,14 In addition to those measures summarized above, other commonly used measures are included (but are not limited to) those listed in this link. View additional measures.
Individual domain-specific disease outcome measures
Use of individual domain-specific measures allows for accurate assessment of disease activity in each domain3
- These measures can be useful to supplement composite measures, particularly where one or two disease manifestations present with severe symptoms, and a composite measure may “dilute” the impact seen in individual domains3
- They can provide an assessment of often overlooked symptoms, such as fatigue, which can have an important impact on a patient’s life13
Many domain-specific measures have been developed and their use in clinical practice depends on several factors, such as individual patient needs, time available, and ease of use.2
For example, there are specific measures available for nail psoriasis (NAPSI), dactylitis (LDI), enthesitis (LEI and the SPARCC index), and psoriasis (PASI).14,*
*Examples of commonly used disease measures and not an exhaustive list of all available measures.

LECTURE SERIES WITH DR. ALEXIS OGDIE
Examine 5 common domain-specific outcome measures for PsA
Join Dr. Alexis Ogdie as she explains the strengths and weaknesses of 5 different outcome measures that are designed to assess a specific aspect of PsA disease, and how they can be used in clinical practice.
Nail Psoriasis Severity Index (NAPSI)
NAPSI is a tool to assess severity of nail psoriasis on the nail bed and nail matrix.14 Evaluations include: onycholysis; splinter hemorrhages; hyperkeratosis; oil-drop dyschromia (for nail bed); and pitting, leukonychia, crumbling, and red spots in the lunula (for nail matrix).14
Considerations
- A simple, numeric, reproducible, objective tool14
- A shorter, modified version, mNAPSI, is available14,15
- Evidence of nail psoriasis can be a surrogate marker for DIP arthritis16
DIP=distal interphalangeal.
Leeds Dactylitis Index (LDI)
LDI measures the severity of dactylitis by assessing the circumference of swollen digits at the base of the finger and tenderness of affected fingers (and toes).14
Considerations
- Total administration takes <10 minutes, with no discomfort to the patient14
Leeds Enthesitis Index (LEI)
LEI measures the presence or absence of tenderness in 6 entheseal sites, developed specifically for use in PsA.14
Considerations
- Takes ~30 seconds to complete, with minimal burden to the patient14
- Routine assessments of entheses with LEI can define enthesitis, a key indicator of disease activity in patients with PsA18
Spondyloarthritis Research Consortium of Canada (SPARCC)
SPARCC measures the presence or absence of tenderness in 16 entheseal sites.14
Considerations
- Takes ~2–5 minutes to complete, with minimal burden to the patient14
- Routine assessments of entheses with SPARCC can define enthesitis, a key indicator of disease activity in patients with PsA18
Psoriasis Area and Severity Index (PASI)
PASI assesses psoriasis lesion burden based on BSA involvement and degree of severity of erythema, induration, and desquamation, for 4 body areas (head, upper and lower extremities, and trunk).14
Considerations
- Not typically used in patients with <3% BSA lesional involvement14
- BSA calculators can be used for scoring14
- Can be performed adequately by trained rheumatologists14
- Extensively studied and validated measure of psoriasis severity2,14
BSA=body surface area
Additional disease outcome measures in PsA
PsA is a highly heterogeneous disease and, as a result, a large array of disease outcome measures have been developed and validated to define and monitor it.2,14 These include physician- and patient-administered measures, composite and single-domain measures for each of the disease domains, and measures for quality of life and ability to carry out activities of daily living.2,14 In addition to those measures summarized above, other commonly used measures are included (but are not limited to) those listed in this link. View additional measures.
Where do we go from here?
Routine implementation of more stringent measures of PsA disease activity is needed to bring clarity to the complexity of PsA disease management and to help raise the bar in helping more patients achieve optimal disease outcome goals.6,20
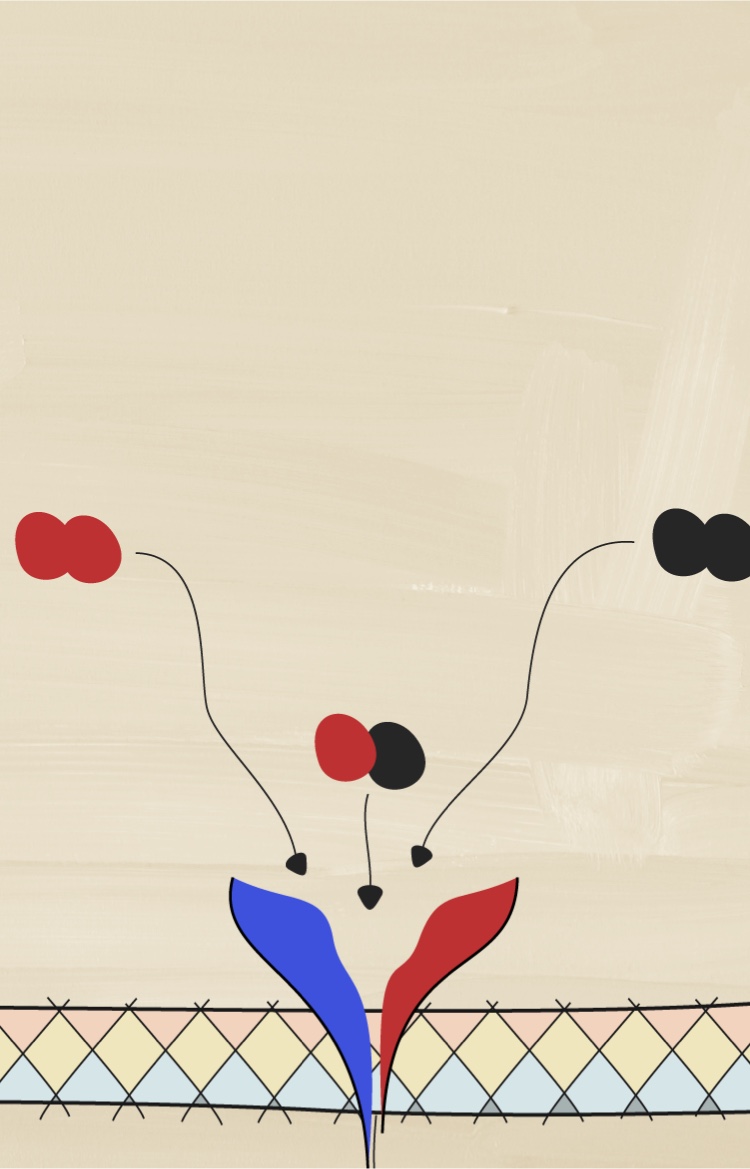
How may a deeper understanding of cytokines help with assessing disease activity?
Understanding the pathologic processes leading to PsA is important to understanding its heterogeneous nature.


NEXT: TAKE THE AXSPA TOUR
Pathobiology overview and the role of cytokines in axSpA
You have finished the PsA tour. Be sure to visit the axSpA tour and discover how several different cytokines have distinct roles in driving inflammation in axSpA.
PREVIOUS ROOM
Setting higher goals
Become a member of the RheuMuseum and be the first to know about new exhibits
- Coates LC, Soriano ER, Corp N, et al. Group for research and assessment of psoriasis and psoriatic arthritis (GRAPPA): updated treatment recommendations for psoriatic arthritis 2021. Nat Rev Rheumatol. 2022;18(8):465-479
- Ogdie A, Coates LC, Mease P. Measuring outcomes in psoriatic arthritis. Arthritis Care Res. 2020;72(Suppl 10):82-109
- Tillett W, McHugh N, Orbai AM, et al. Outcomes of the 2019 GRAPPA workshop on continuous composite indices for the assessment of psoriatic arthritis and membership-recommended next steps. J Rheumatol Suppl. 2020;96:11-18
- Orbai AM, de Wit M, Mease P, et al. International patient and physician consensus on a psoriatic arthritis core outcome set for clinical trials. Ann Rheum Dis. Apr 2017;76(4):673-680. doi:
- Tucker LJ, Coates LC, Helliwell PS. Assessing disease activity in psoriatic arthritis: a literature review. Rheumatol Ther. 2019;6(1):23-32
- Coates LC, FitzGerald O, Merola JF, et al. Group for research and assessment of psoriasis and psoriatic arthritis/outcome measures in rheumatology consensus-based recommendations and research agenda for use of composite measures and treatment targets in psoriatic arthritis. Arthritis Rheumatol. 2018;70(3):345-355
- Smolen JS, Schöls M, Braun J, et al. Treating axial spondyloarthritis and peripheral spondyloarthritis, especially psoriatic arthritis, to target: 2017 update of recommendations by an international task force. Ann Rheum Dis. 2018;77(1):3-17
- Schoels MM, Aletaha D, Alasti F, et al. Disease activity in psoriatic arthritis (PsA): defining remission and treatment success using the DAPSA score. Ann Rheum Dis. 2016;75(5):811-818
- Gossec L, McGonagle D, Korotaeva T, et al. Minimal disease activity as a treatment target in psoriatic arthritis: a review of the literature. J Rheumatol. 2018;45(1):6-13
- Wervers K, Vis M, Tchetveriko I, et al. Burden of psoriatic arthritis according to different definitions of disease activity: comparing minimal disease activity and the disease activity index for psoriatic arthritis. Arthritis Care Res. 2018;70(12):1764-1770
- Gossec L, de Wit M, Kiltz U, et al. A patient-derived and patient-reported outcome measure for assessing psoriatic arthritis: elaboration and preliminary validation of the psoriatic arthritis impact of disease (PsAID) questionnaire, a 13-country EULAR initiative. Ann Rheum Dis. 2014;73(6):1012-1019
- Di Carlo M, Becciolini A, Lato V, et al. The 12-item psoriatic arthritis impact of disease questionnaire: construct validity, reliability, and interpretability in a clinical setting. J Rheumatol. 2017;44(3):279-285
- Tillett W, Dures E, Hewlett S, et al. A multicenter nominal group study to rank outcomes important to patients, and their representation in existing composite outcome measures for psoriatic arthritis. J Rheumatol. 2017;44(10):1445-1452
- Mease PJ. Measures of psoriatic arthritis: Tender and swollen joint assessment, psoriasis area and severity index (PASI), nail psoriasis severity index (NAPSI), modified nail psoriasis severity index (mNAPSI), mander/Newcastle enthesitis index (MEI), Leeds enthesitis index (LEI), spondyloarthritis research consortium of Canada (SPARCC), Maastricht ankylosing spondylitis enthesis score (MASES), Leeds dactylitis index (LDI), patient global for psoriatic arthritis, dermatology life quality index (DLQI), psoriatic arthritis quality of life (PsAQOL), functional assessment of chronic illness therapy-fatigue (FACIT-F), psoriatic arthritis response criteria (PsARC), psoriatic arthritis joint activity index (PsAJAI), disease activity in psoriatic arthritis (DAPSA), and composite psoriatic disease activity index (CPDAI). Arthritis Care Res. 2011;63 Suppl 11:S64-85
- Cassell SE, Bieber JD, Rich P, et al. The modified Nail Psoriasis Severity Index: validation of an instrument to assess psoriatic nail involvement in patients with psoriatic arthritis. J Rheumatol. 2007;34(1):123-129
- Lai TL, Pang HT, Cheuk YY, et al. Psoriatic nail involvement and its relationship with distal interphalangeal joint disease. Clin Rheumatol. 2016;35(8):2031-2037
- Mease PJ, Smolen JS, Behrens F, et al. A head-to-head comparison of the efficacy and safety of ixekizumab and adalimumab in biological-naïve patients with active psoriatic arthritis: 24-week results of a randomised, open-label, blinded-assessor trial. Ann Rheum Dis. 2020;79(1):123-131
- Kristensen S, Christensen JH, Schmidt EB, et al. Assessment of enthesitis in patients with psoriatic arthritis using clinical examination and ultrasound. Muscles Ligaments Tendons J. 2016;6(2):241-247
- Strober B, Karki C, Mason M, et al. Impact of Psoriasis Area and Severity Index (PASI) on patient reported outcomes in patients with psoriasis: Results from the Corrona Psoriasis Registry. American Academy of Dermatology Annual meeting 2017, Orlando, FL. Poster number 4405
- Dures E, Hewlett S, Lord J, et al. Important treatment outcomes for patients with psoriatic arthritis: a multisite qualitative study. Patient. 2017;10(4):455-462