

Examine the burden of disease of PsA
The prevalence of comorbidities in patients with PsA
PsA is frequently associated with comorbidities that could affect the disease outcome and can impact a patient’s daily functioning and quality of life.1,2 To optimize important patient outcomes, physicians should globally assess disease activity and consider the impact of comorbidities on management decisions.1
Common comorbidities in patients with PsA include:

LECTURE SERIES WITH DR. SAAKSHI KHATTRI
The art of assessing the multiple disease domains of PsA and common comorbidities
Join Dr. Khattri as she discusses the complexity of managing patients with PsA who are experiencing comorbidities and multiple-domain involvement, and why a multidisciplinary approach is needed.
Recognizing the total burden of disease of PsA
PsA has a negative impact on patients’ quality of life, across all disease domains. For example:
- Patients with enthesitis and dactylitis report increased disability from reduced physical functioning, as well as increased sleep disturbances and fatigue6,9,10
- Patients report itching at the location of skin involvement in psoriasis, and pain/swelling of joints as factors contributing the most to disease severity11
- Nail disease and disfiguration have been associated with physical and emotional distress and decreased productivity at work6
The quality of life for patients with PsA is further reduced by experiencing clinical presentations across multiple disease domains, comorbidities, and increased disease severity.12
It is important to consider all aspects of disease activity when managing patients with PsA—from specific measures of the various disease domains to assessing the impact on a patient’s quality of life.1,2
Explore the disease outcome measures used for PsA in our exhibit
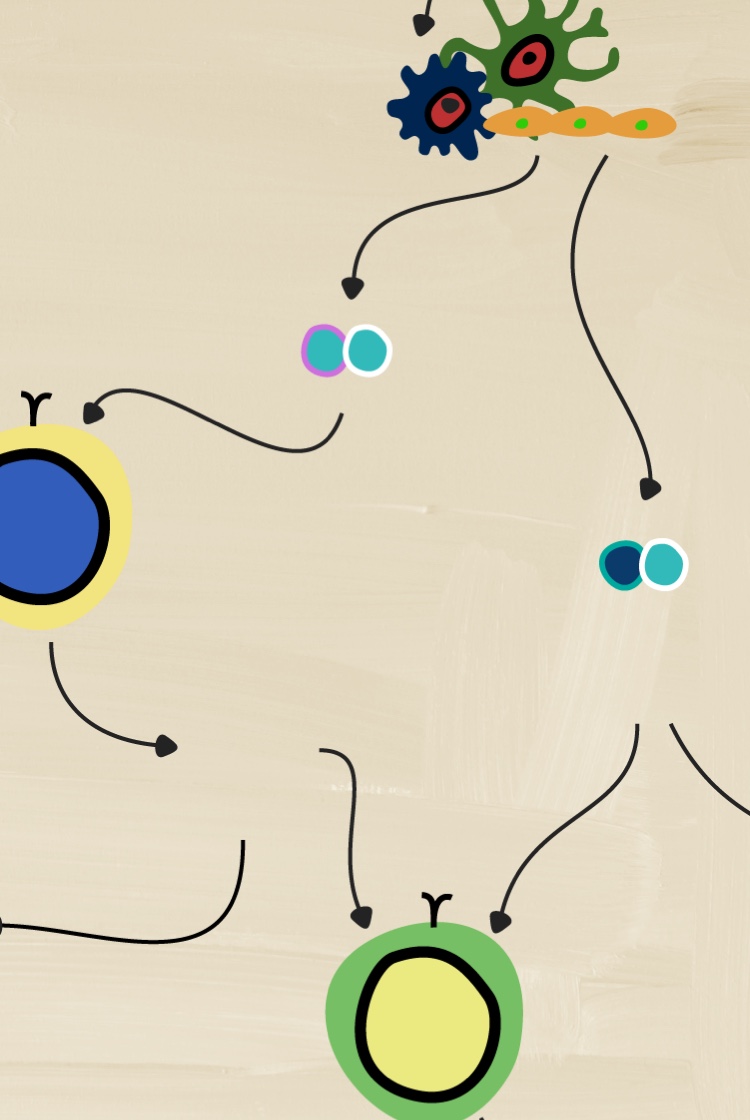

How can underlying causes of disease affect the burden to patients?
A deeper understanding of the pathological processes that cause certain disease manifestations may impact patients’ burden of disease.


NEXT EXHIBIT IN THE PSA TOUR
PsA outcomes
Explore different disease outcome measures and their importance in defining PsA disease activity in clinical practice.
PREVIOUS ROOM
Clinical manifestations
Become a member of the RheuMuseum and be the first to know about new exhibits
- Lubrano E, Scriffignano S, Belen Azuaga, A, et al. Impact of Comorbidities on Disease Activity, Patient Global Assessment, and Function in Psoriatic Arthritis: A Cross-Sectional Study. Rheumatol Ther. 2020;7:825-836. doi.org/10.1007/s40744-020-00229-0
- Gupta S, Syrimi Z, Hughes DM, et al. Comorbidities in psoriatic arthritis: a systematic review and meta-analysis. Rheumatol Int. 2021;41:275–284. doi.org/10.1007/s00296-020-047
- Husted JA, Thavaneswaran A, Chandran V, et al. Incremental effects of comorbidity on quality of life in patients with psoriatic arthritis. J Rheumatol. 2013;40(8):1349-1356. doi:10.3899/jrheum.121500
- Tam LS, Tomlinson B, Chu TT, et al. Cardiovascular risk profile of patients with psoriatic arthritis compared to controls--the role of inflammation. Rheumatology (Oxford). 2008;47(5):718-723. doi:10.1093/rheumatology/ken090
- Dal Bello G, Gisondi P, Idolazzi L, et al. Psoriatic arthritis and diabetes mellitus: a narrative review. Rheumatol Ther. 2020;7(2):271-285. doi:10.1007/s40744-020-00206-7
- Lee S, Mendelsohn A, Sarnes E. The burden of psoriatic arthritis: a literature review from a global health systems perspective. P T. 2010;35(12):680-689.
- Raychaudhuri SK, Chatterjee S, Nguyen C, et al. Increased prevalence of the metabolic syndrome in patients with psoriatic arthritis. Metab Syndr Relat Disord. 2010;8(4):331-334. doi:10.1089/met.2009.0124
- Magrey MN, Antonelli M, James N, et al. High frequency of fibromyalgia in patients with psoriatic arthritis: a pilot study. Arthritis. 2013;2013:762921. doi:10.1155/2013/762921
- Kaeley GS, Eder L, Aydin SZ, Gutierrez M, et al. Enthesitis: A hallmark of psoriatic arthritis. Semin Arthritis Rheum. 2018;48(1):35-43. doi:10.1016/j.semarthrit.2017.12.008
- Kavanaugh A, Helliwell P, Ritchlin CT. Psoriatic arthritis and burden of disease: patient perspectives from the population-based multinational assessment of psoriasis and psoriatic arthritis (MAPP) survey. Rheumatol Ther. 2016;3(1):91-102. doi:10.1007/s40744-016-0029-z
- Lebwohl MG, Bachelez H, Barker J, et al. Patient perspectives in the management of psoriasis: results from the population-based Multinational Assessment of Psoriasis and Psoriatic Arthritis Survey. J Am Acad Dermatol. 2014;70(5):871-881.e830. doi:10.1016/j.jaad.2013.12.018
- Ogdie A, Hur P, Liu M, et al. Effect of multidomain disease presentations on patients with psoriatic arthritis in the corrona psoriatic arthritis/spondyloarthritis registry. J Rheumatol. 2021;48(5):698-706. doi:10.3899/jrheum.200371